The COVID-19 pandemic has upended lives in many ways over the last 15 months (and counting!).
17 June 2021
As of June 15, 2021 there have been 176 million confirmed cases and 3.8 million deaths worldwide. The crisis has led to significant changes at hospitals, both for services offered and for patients’ willingness to visit. One area of particular importance is the reduction in the number of cancer screenings.
As hospitals around the world were admitting record numbers of patients who were infected with COVID-19, many other procedures were delayed or outright cancelled as resources were consumed by the pandemic. Cancer services, including screenings, have reduced materially over the pandemic as some have been classified as lower-priority and patients, concerned about exposure to COVID-19 in the hospitals, have been more reluctant to attend.
A November 2020 US Study used data from a large medical claims clearinghouse to gain insights into the impact of COVID-19 on the US cancer population. One of the main results from the study was a significant year over year decrease in cancer screenings, visits, therapy, and surgeries. The study used a baseline period of March-July 2019 and compared that to March-July 2020 for four different types of cancer. At the peak of the first pandemic wave, screenings were lower by 85%, 75%, 74%, and 56% for breast, colon, prostate, and lung cancers respectively.
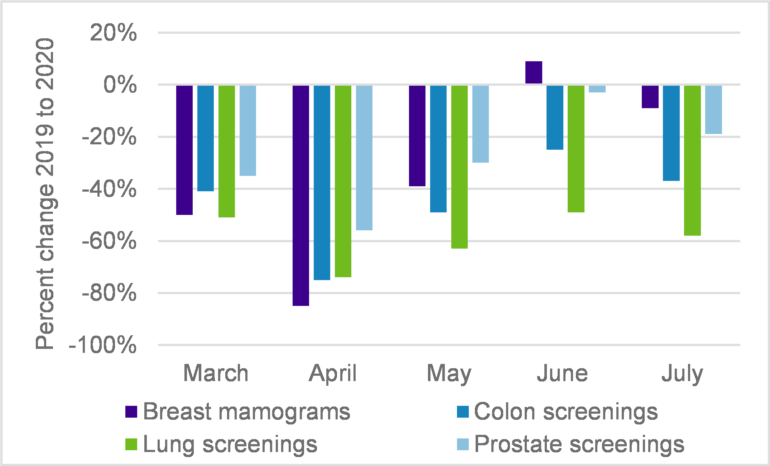
Source: https://pubmed.ncbi.nlm.nih.go...
A Canadian Cancer Survivor Network survey found that 54% of cancer patients had their cancer care appointments rescheduled, postponed, or cancelled because of COVID-19. For pre-diagnosis or recently diagnosed patients, the number was higher at about 75%.
Impacts of delaying screenings
It may not be surprising that the earlier cancer can be detected in a person, the higher the odds of survival and the higher the person’s remaining life expectancy. Experts say that, in general, cancers are easier to treat in their early stages and delays in screening could mean cancers are larger and more advanced before they are detected.
A July 2020 UK modelling study estimated that COVID-19’s impact on cancer would cause an increase of 7.9%-9.6% breast cancer deaths up to 5 years after diagnosis. It showed similar increases for other cancer types such as colorectal (15.3%-16.6%), lung (4.8%-5.3%), and oesophageal (5.8%-6.0%).
A November 2020 meta-study in the US looked at seven different cancer types (bladder, breast, colon, rectum, lung, cervical, and head and neck) and investigated the impact on mortality for delays in treatment. It determined that for every 4-week delay in cancer treatments, mortality increased materially for all cancer types, from 1%-6% for lung cancer up to around 23% for cervix cancer.
Delays will likely get worse before they get better
The research into cancer delays to date has understandably focused on the first COVID-19 wave. Countries such as the US, UK, and Canada have also experienced second and third waves, which have continued to take their toll on healthcare systems resulting in additional delays for cancer screenings and treatments creating more backlogs in the system.
How long might it take to clear the backlog and “catch up” to where we could have been without COVID-19? Demand for cancer-related services will go up as people make up missed appointments, many joining at more advanced cancer stages. How long will it take for the already taxed healthcare systems to get back to pre-pandemic levels of service and then ramp up to meet additional demand? Aging populations, already driving up demand, will put further pressure on the systems.
What does this mean for pension plans and insurers?
The impact of the COVID-19 pandemic on society may be felt for many years. Excess deaths (i.e., those above expected) in 2020 hit historic highs: US (+14.8%), UK (+13.5%), and Canada (+6.5%). The direct impact for pension plans and insurers has not yet been quantified as the general population impact of COVID-19 could be different than for pensioner populations.
As mentioned, there will be long term effects of delays in cancer screenings with experts modelling the increased mortality to go beyond 2030 and increase over time. Statistics Canada data identified improvements in cancer treatments as a material driver of longevity improvements for younger pensioners (i.e., those aged 65-74) who tend to have the largest liabilities (see opposite chart), so this could result in material impact to pension plan liabilities.
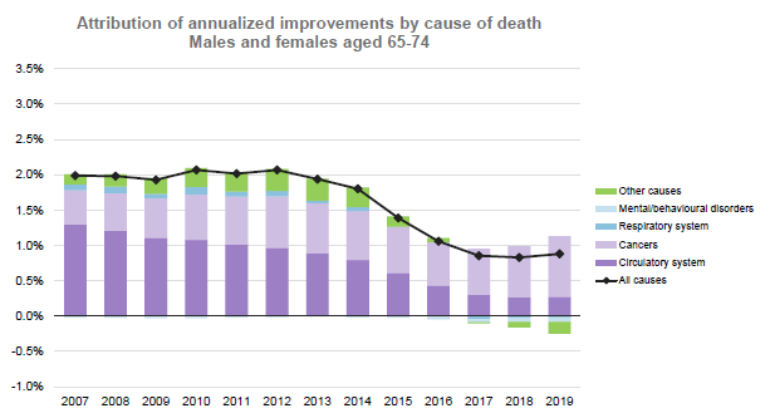
Source: Club Vita analysis based on Statistics Canada data. Table 17-10-0005-01 Population estimates on July 1st, by age and sex
Could the additional mortality due to cancer screening delays result in some “lost years” of longevity improvements or even negative improvements (i.e., reductions in life expectancy)? If so, how long could this last? And would this impact be felt evenly across different socio-economic groups?
Only time will tell how this will unfold across both the general and pensioner populations. Club Vita has created its own COVID-19 longevity scenarios to assist Club members in understanding and quantifying potential future scenarios for the US, UK, and Canada. Pension plans and insurers will need to continually monitor and adjust their expectations as experience emerges.
Need more information?
If you have any further questions our team would be happy to help you.



